
Enquiry Form.
Please complete and we will call you back.
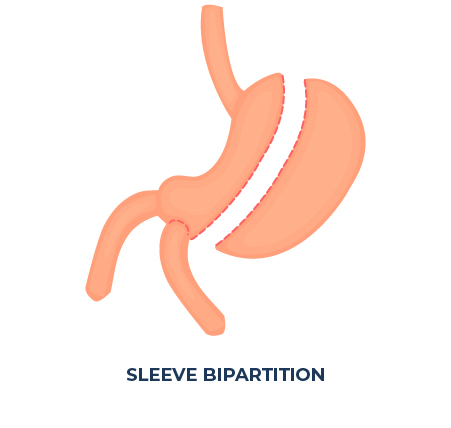
What is a Sleeve Bipartition Bypass?
Sleeve bipartition is also called modified Roux-en-Y gastric bypass.
During the procedure, the stomach is sleeved and a hole in the stomach wall, close to the pylorus, is made. This hole in the stomach wall called the second stomach exit is connected to a shortened section of the small intestine that allows the food to go more quickly into the large intestine. The rest of the intestine is then reconnected to the “bypassed” section, so that a portion of the food will still go through the pylorus and the entirety of the intestine.
From its first iteration in 1950, bypass surgery has been improved year after year. Even today, we keep finding better methods and tools to satisfy and improve on all requirements of the surgery: weight loss results, speed of recovery, comfort, long-term sustainability, etc. This version of the gastric bypass was invented in 2004 in Brazil by Dr. Sergio Santoro.
 1300 190 461
1300 190 461



 Penrith Consulting Rooms
Penrith Consulting Rooms